BLOG
Ambulance Costs After a New Jersey Car Crash
 Being involved in a car crash is a traumatic experience that catches most of us off guard. At the accident scene, getting immediate medical care is critical. Sometimes this could mean being transported by ambulance to the nearest hospital.
Being involved in a car crash is a traumatic experience that catches most of us off guard. At the accident scene, getting immediate medical care is critical. Sometimes this could mean being transported by ambulance to the nearest hospital.
Who pays for emergency ambulance transportation services after a crash? Will you have to pay for it or do those costs get paid for by the insurance of the at-fault driver?
In the article below, Lynch Law Firm, PC discusses who foots the bill for emergency ambulance transportation and other crucial medical services after a New Jersey collision.
Need legal help today? Our team of knowledgeable New Jersey auto accident lawyers has been helping injured crash victims for decades. Find out if you have a case – there is no cost to you.
Health Insurance and Auto Insurance: New Jersey’s Dual Safety Net
Since New Jersey is a no-fault state , you must initially seek medical coverage under your own insurance. This includes ambulance services. That said, you may have two primary sources of available coverage: your health insurance and auto insurance.
Health insurance is a safety net that goes beyond the circumstances of a crash. Regardless of how you were injured, the purpose of health insurance is to cover your medical costs, including ambulance services.
Personal Injury Protection (PIP) provides another layer of insurance. If you own and drive a car in New Jersey, you must purchase this coverage as part of your overall auto insurance policy. PIP insurance provides immediate coverage for your ambulance services and other medical treatments, no matter who was at fault for the crash.
Which Insurance Applies First After a Car Crash?
You can choose to have your health insurance as the first point of coverage for your car crash medical costs, including your ambulance services. Be careful, however, as some health insurers do not include coverage for any injuries caused by a car accident.
Every insurance plan is different, so it is a good idea to check with your provider ahead of time to see what is covered and when. It is much easier to plan these things in advance. Trying to figure your coverage out right after a crash while dealing with injuries only adds to your immediate stress.
If Your Health Insurance Covers Medical Costs After a Car Crash
If your health insurance covers injuries resulting from car crashes, remember you will still have to pay the out-of-pocket deductibles and co-pays outlined in your plan. In this situation, your insurance should cover the costs of your ambulance ride if it is medically necessary.
How Do I Choose Health Care as My Primary Coverage After a Crash?
The first step is to be sure your health insurance covers injuries from traffic accidents. If it does, then you can choose it as your first point of coverage after a crash. Simply contact your auto insurer to add it to your policy. One precaution if you do this – be sure to remove this option if your health insurance gets canceled for any reason.
What if Your Health Insurance Does Not Pay
If your health insurance plan does not cover collisions, then your PIP insurance will. PIP insurance pays for your ambulance transportation, emergency room visit, diagnostic testing and more. However, there are two caveats. First, PIP only pays up to the limits of the policy you purchased, and second, you still have to pay the initial out-of-pocket cost of the deductible you selected.
In New Jersey, PIP deductibles range from $250 to $2,500. Under a standard policy, the minimum PIP coverage is $15,000 per person and $30,000 per accident. The minimum coverage does not go very far, which is why many drivers opt to increase that coverage to $250,000. Now might be a good time to review what coverage you have to make sure your insurance meets your current needs.
What if Payment for My Ambulance Transport is Denied?
The main reason an ambulance claim may get denied is if the service was considered medically unnecessary. Does this mean you should refuse treatment at the scene of a crash? Absolutely not. Your health should always be your priority.
Crash victims are often in no state to decide for themselves whether they need an ambulance transport or not. Emergency medical technicians (EMTs) at the crash scene, however, are trained to determine when ambulance services are medically necessary.
A denied ambulance claim is just one example of how you can benefit from having a knowledgeable attorney manage your case. An attorney will know how to dispute this denial and will fight to protect your interests.
Call Our Trusted Law Firm for Legal Help
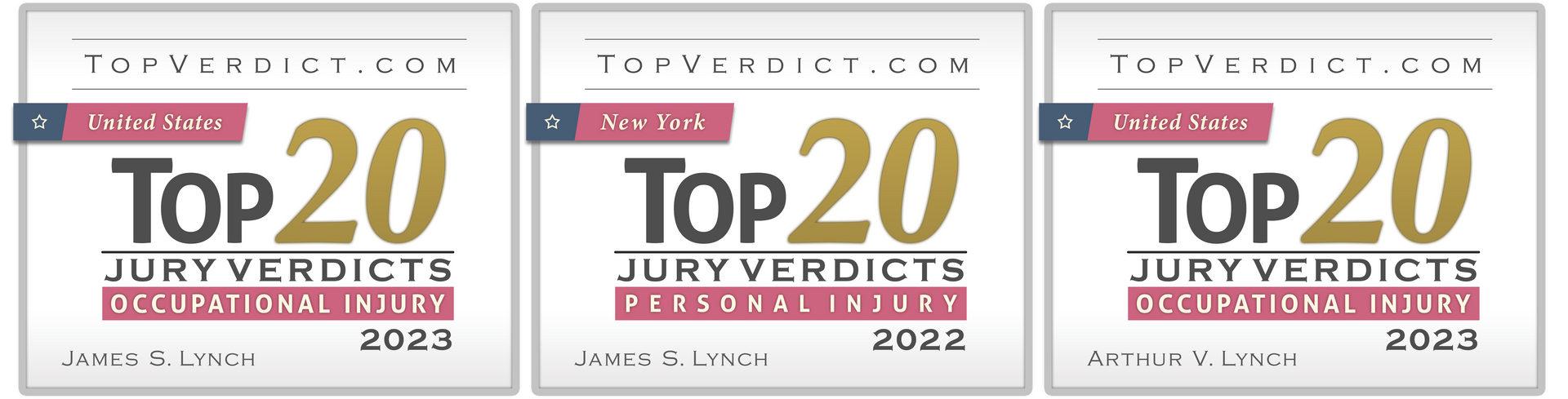
At Lynch Law Firm, PC, we have the resources and staff to help you after a crash that caused your injuries and resulted in medical bills and other losses. While we can never guarantee a dollar amount, we have a proven history of success. We always strive to recover full and fair compensation for your damages, including the costs of your ambulance transport services.
The good news is that you can find out if you have a case with no cost or obligation. If you have a case and choose our firm to represent you, there are no out-of-pocket costs or fees to pay. We only get paid if we win a settlement or jury-awarded verdict on your behalf.
Experienced Lawyers. Proven Results. Call (800) 518-0508 today.